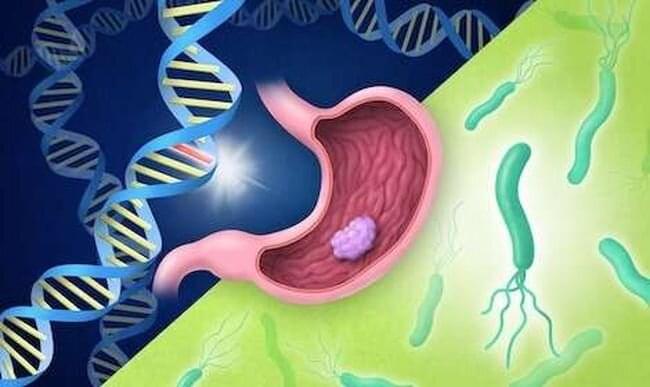
A large case-control study by international researchers at the RIKEN Center for Integrative Medical Sciences (IMS) in Japan has found that people who carry certain genetic risk factors for gastric (stomach) cancer have a much greater risk if they have also been infected by the bacterium Helicobacter pylori. The study, published in The New England Journal of Medicine, could contribute to the development of tailored genomic medicine for treating stomach cancer.
Stomach cancer is the fourth leading cause of cancer death worldwide and has both environmental and genetic risk factors. Environmentally, infection by H. pylori increases the risk of stomach cancer. Because the virulence of H. pylori in East Asia is high, the incidence of stomach cancer is higher in countries like Japan. Genetically, while hereditary gene variation is why we have different colored eyes and are unique as individuals, sometimes gene variants are associated with the risk of disease. For example, individuals who carry a certain hereditary pathogenic variant of the CDH1 gene have an increased risk of gastric cancer.
Testing for the presence of pathogenic variants is now one of several measures being taken for cancer prevention, surveillance, and treatment selection. However, because large-scale, case-control studies are lacking, and because those that exist have not assessed how the risk for stomach cancer changes when pathogenic variants interact with environmental factors like H. pylori, it remains unclear what actual clinical measures can be taken. To address this issue, researchers therefore evaluated the risk of gastric cancer in a large case-control study of Japanese people, considering whether they were carriers of pathogenic variants and whether they had been infected by H. pylori.









Leave a reply